Surgical site infections are the 3rd most frequently reported hospital-acquired infections
Definition
Surgical site infections (SSIs) can occur after surgery in the part of the body where the surgery took place. An SSI typically occurs 30 days after surgery (that does not involve implants), but can occur within 1 year if an implant is placed and infection appears to be related to surgery.
SSI’s account up to 20%-25% of all hospital-acquired infections. They are associated with longer hospital stays, additional surgical procedures, treatment in ICUs and high mortality rate.
SSIs can result from all kinds of surgery, including from anastomotic leak (AL); uncontrolled SSI can result in sepsis, a risk for most types of uncontrolled infection.
Causal Agents
SSIs are caused by bacteria that enter through surgical incisions, either from endogenous (i.e. present on patient’s skin or at surgical site) or exogenous (from surgical instruments, operating room surfaces, air, etc.) sources
Types of SSI
Incisional SSI
Superficial incisional: Involves skin only
Deep incisional: Infection occurs beneath the incision area in muscle and tissues
Organ/organ space SSI
Infection involving any part of the anatomy in organs and spaces other than the incision, which was opened or manipulated during operation
Source: Iskandar K et al 2019, Infectious Disease Advisor, Jenks PJ et al 2014, Zimlichman E et al 2013, Financial Impact of Surgical Site Infections 2018, Shephard J et al 2013, PSNet AHRQ, 2019 Covira Surgical: Confidential Information Memorandum
Organ Infection
Wound Infections
Anastomotic leak is one of the most serious complications following any type of gastrointestinal anastomotic surgery
Definition
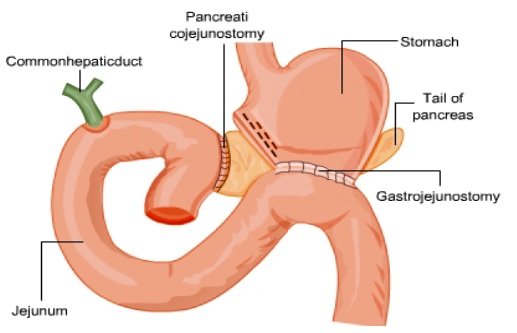
Anastomotic leak (AL), the result of a union leading to a leakage of, is most commonly observed in gastrointestinal surgeries (colorectal anastomotic leak, CAL), where the intestinal wall loses integrity at the surgical junction, leading to leakage Complications from AL can include fever and pain, with the potential for severe sepsis and multi-organ failure or death.
Risk Factors (Non-exhaustive)
Patient factors: Diabetes, obesity, malnutrition, smoking, alcohol consumption
Medication: The use of corticosteroids or some immunosuppressants
Surgical factors: Longer intra-operative time, peritoneal contamination (pus, feces etc.)
Bacteria as a root cause
In response to stress caused by surgery, the patient releases inflammatory and other compensatory signals, leading to local environmental change to which the local microbes respond.
The response, driven by loss of local phosphate, leads to phenotypic changes that promote virulence and further microenvironment breakdown.
Sources: Internal presentation; Schardey HM et al. 2017; Russ AJ and Casillas MA 2016; Gaines S et al. 2018; Michael J et al.2018 Covira Surgical: Confidential Information Memorandum
Sepsis is a life threatening condition caused
by the body’s response to an infection
Definition
Sepsis is a life-threatening medical emergency leading to organ dysfunction due to dysregulated host response to infection.
Sepsis results from the runaway host response to an infection triggering a chain reaction throughout the body. Without timely treatment, sepsis can rapidly lead to tissue damage, organ failure and death.
In the USA, sepsis is the most common cause of in-hospital deaths and costs more than $24Bn annually.
Causal Agents
Any infection can trigger sepsis, but the following are more likely to cause sepsis: pneumonia, abdominal infection, kidney infection, bloodstream infection.
Incidence
The number of sepsis cases in the US are increasing due to the following factors:
Increases in antibiotic resistance
Aging population
Increase in number of people with compromised immune systems
Source: CDC.GOV, Healthline Covira Surgical: Confidential Information Memorandum